- 39 New London Turnpike Suite 120 Glastonbury, CT 06033

‘Subconcussive’ is a Dangerous Misnomer: Hits of Greater Magnitude than Concussive Impacts May Not Cause Symptoms
British Journal of Sports Medicine
July 1, 2024; Vol. 58; No. 14; pp. 754-756
Christopher J Nowinski, Hye Chang Rhim, Ann C McKee, Ross D Zafonte, David W Dodick, Robert C Cantu, Daniel H Daneshvar: from Boston University Chobanian & Avedisian School of Medicine, Harvard Medical School, and Mayo Clinic: This editorial cites 15 references.
HAE = head acceleration events
KEY POINTS FROM THIS EDITORIAL:
1) “Concussion is a traumatic brain injury (TBI) defined by the presence of transient signs and symptoms related to alterations in brain function due to biomechanical force.”
2) “The term ‘subconcussive’ has emerged to refer to both subclinical head acceleration events (HAEs) and injuries (as defined by clinical, biomarker and/or neuroimaging changes).”
3) “When referring to impacts, the prefix ‘sub’ implies lower magnitude HAEs than those that cause a diagnosed concussion.”
4) The authors “suggest replacing subconcussive when referring to injury with ‘subclinical TBI.’”
5) There is no HAE magnitude threshold that would characterize concussion. [Very Important]
6) Football helmet accelerometers “highlight that ‘subconcussive’ impacts are frequently associated with greater head acceleration than concussive impacts.” [Very Important]
7) “Acutely, HAEs without symptoms of concussion have been associated with increasing biomarkers of neuroinflammation, suggesting possible neurological injury.”
8) “Imaging studies have demonstrated that repetitive head impacts in the absence of symptomatic concussion are associated with functional impairment and structural damage to the integrity of brain structures including white matter changes, cortical thinning and volume loss.” [Key Point]
9) “Over time, athletes sustaining non-concussive HAEs may also be at higher risk of concussion.” [Very Important]
10) “In the long-term, cumulative exposure to non-concussive impacts may increase the risks of neurodegenerative disease including amyotrophic lateral sclerosis (ALS) and chronic traumatic encephalopathy (CTE).” [Very Important]
11) “Duration of exposure to non-concussive HAEs has been described as being higher in professional football players with ALS compared with those without, and in predicting both CTE status and severity whereas concussion does not.”
12) “The observation that some non-concussive impacts can have clinical implications is unsurprising given the widely accepted evidence that subclinical injury can lead to neurological deficits in other disease processes, such as how some ischaemic events can lead to subclinical cerebrovascular disease that can accumulate and eventually manifest as dementia and cognitive decline.”
13) “[It is] possible that sensory obtundation [a dulled or reduced level of alertness or consciousness] has occurred in some individuals exposed to TBI, further weakening the link between TBI and symptoms.”
14) “The term ‘subconcussive’ should be retired when referring to both impacts and injuries.”
15) “The absence of symptoms following an HAE does not indicate that no injury occurred, but rather that no injury occurred to a salient network; it is possible that damage occurred in an area that is not responsible for conscious processes.” [Key Point]
16) “There are differences in how individuals respond to the same head impact based on unique differences in brain anatomy, premorbid risk factors and comorbid conditions, which can lead to differences in subsequent injury risk.” [Key Point]
COMMENTS FROM DAN MURPHY
Our office now uses subclinical TBI and no longer uses subconcussive (blow/injury) in our charting and reports.
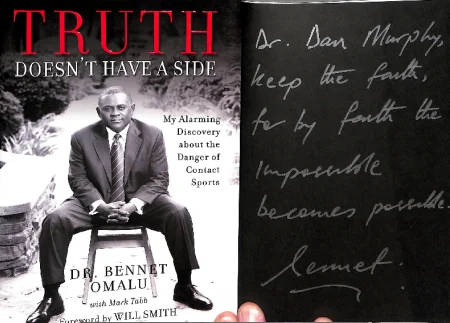
The most important point in this article is the emphasis that repetitive subclinical TBI leads to both injury and significant deleterious long-term sequalae for the brain. This is the theme of the movie “Concussion” and of the book (Truth Does Not Have a Side) by the nonfictional character physician/pathologist Bennet Omalu (attached). It is also the theme of the book Damage (also attached). We have reviewed these articles that support this study:
Article Review 31-17:
Mixed Pathologies Including Chronic Traumatic Encephalopathy Account for Dementia in Retired Association Football (soccer) Players
Article Review 38-17: First-Time Sports-Related Concussion Recovery
Article Review 49-22:
Outcomes in Patients with Mild Traumatic Brain Injury Without Acute Intracranial Traumatic Injury
Article Review 7-24:
Long-term Patterns of Change Following Traumatic Brain Injury

39 New London Turnpike Suite 120
Glastonbury, CT 06033
